2. Apply Baby Powder Under the Halo Vest to Prevent Irritation.
- Research article
- Open Admission
- Published:
Function of O-C2 angle in the development of dysphagia in patients with halo-vest fixation
BMC Musculoskeletal Disorders book 21, Article number:131 (2020) Cite this article
Abstract
Background
Dysphagia is one of the nearly serious complications in patients treated with a halo-vest brace. However, the crusade of dysphagia development by halo-vest fixation is not notwithstanding articulate. We therefore investigated the incidence of dysphagia and cervical alignment as well as clinical data from medical charts in patients treated with a halo-vest brace.
Methods
Nosotros retrospectively reviewed clinical data from the medical charts of 49 patients who had undergone halo-vest fixation. Occipito (O)-C2 angle, C2-C6 bending, and pharyngeal inlet angle were assessed by lateral patently X-rays of the cervical spine. The impacts of these parameters on incidence and severity of dysphagia were analyzed.
Results
13 patients (32%) suffered from dysphagia during halo-vest fixation, and age and length of intensive care unit (ICU) stay were greater in the dysphagia group (p = 0.044 and 0.013, respectively) than in those who did not develop dysphagia. O-C2 angle was smaller in the dysphagia grouping (p = 0.016). Later on multivariate logistic analysis, body mass index, ICU stay, and O-C2 angle remained as independent risk factors related to incidence of dysphagia. Spearman rank correlation showed a negative correlation between ICU stay and Food Intake Level Calibration (FILS) (p = 0.026), and a positive correlation betwixt O-C2 bending and FILS (p = 0.008).
Conclusion
This written report suggested that O-C2 angle is related to both incidence and severity of dysphagia due to halo-vest fixation.
Background
As a role of the handling class for cervical spine fracture and/or spinal cord injury, cervical orthoses are required to immobilize cervical vertebrae. Among cervical orthoses, the halo-belong brace provides the greatest fixation of the head and neck [1, two]. The halo-vest has been a common tool for immobilization of the cervical spine since its evolution in 1959 by Perry and Nickel [3]. Still, complications such as pin loosening and infection have been reported in patients fixed using the halo-vest caryatid [2].
Among the complications with the halo-vest brace, dysphagia is i of the well-nigh serious, leading to life-threatening aspiration pneumonia, especially in elderly patients [ii, 4]. Morishima et al. [5] establish that halo-vest fixation with unnatural alignment acquired dysphagia in normal, healthy volunteers. Bradley et al. [vi] found that a longer stay in the intensive care unit (ICU) was associated with the incidence and severity of dysphagia in traumatically injured patients treated with a halo-belong brace. Although they analyzed various factors from medical charts, including severity of injury, length of ICU stay, elapsing of ventilator utilize and length of hospital stay, the status of cervical alignment was not evaluated in that study.
In patients who have undergone cervical fusion, accumulating evidence suggests that cervical alignment provides a predictor of postoperative dysphagia [seven,8,nine,10,11,12,xiii,14,15,16,17,18]. With occipitocervical fusion, the subtract in O-C2 angle is a predictor of dysphagia after surgery [7,viii,nine,10,11,12,13,14,15,sixteen]. The decrease in O-C2 bending shifts the mandible posteriorly with the tongue root, resulting in a reduction in the pharyngeal infinite. This backward motion of the natural language root presumably causes oropharyngeal stenosis and damage of adequate motion of the epiglottis. In improver, Kaneyama et al. [19] recently reported the pharyngeal inlet bending (PIA), which besides correlates with pharyngeal space, every bit a predictor of dysphagia in patients who underwent occipitocervical fusion.
On the other mitt, in cervical fusion not involving the cranium, the C2-C7 angle is reported to exist related to dysphagia after surgery [17, 18]. Tian et al. [xviii] reported that deviation from cervical lordosis causes posterior pharyngeal wall bulging, resulting in a reduction in the pharyngeal space.
Taken together, we hypothesized that not only clinical data from medical charts such as length of ICU stay and mechanical ventilation, just also united nations-optimized cervical alignment would bear upon on the incidence of dysphagia in patients with halo-vest fixation. The aim of this written report was to elucidate the relationship between cervical alignment and incidence of dysphagia in patients treated with a halo-belong brace by evaluating lateral radiological findings of the cervical spine, likewise equally patient clinical data from medical charts. Relationships between extracted risk factors and severity of dysphagia were besides analyzed.
Methods
Subjects
We retrospectively reviewed the medical charts of patients who had undergone halo-vest fixation in our constitute between January 2006 and Baronial 2016. Collected clinical data included demographic data and duration of wearing the halo-belong, length of ICU stay, duration of ventilator use, presence or absence of tracheostomy, etiology, presence or absence of surgery for cervical fixation earlier halo-vest fixation, and complications. Patients with severe dementia (Mini-Mental State Examination score < ten), facial trauma, neurodegenerative disease, obvious cognitive infraction, spinal cord injury of grade A or B co-ordinate to the Frankel classification, or confused country (Richmond Agitation-Sedation Calibration below − 2 or above + 2) throughout the period of wearing the halo-vest were excluded from this study.
Dysphagia evaluation
Severity of dysphagia was assessed past Food Intake Level Calibration (FILS) from medical chart descriptions of the eating condition of patients [20]. In our institution, patients with FILS level viii–ten are followed by nurses who belong to each ward, and patients with FILS level one–vii are followed by the institutional team for dysphagia rehabilitation and are appropriately assessed by fiberoptic endoscopic and/or video-fluoroscopic swallow studies. Severity of dysphagia was evaluated within 1 week afterwards halo-belong fixation in a sitting position as far as possible. Based on FILS level, patients were classified into non-dysphagia (FILS level: ten) and dysphagia (FILS level: ane–9) groups. FILS is divers as follows [20]: Level 1, no swallowing training; Level two, swallowing training not using nutrient; Level 3, swallowing preparation using a modest quantity of nutrient; Level 4, easy-to-eat nutrient less than the quantity of a meal, but predominantly with alternative nutrition; Level 5, easy-to-swallow food orally ingested for one–2 meals, but culling nutrition besides given; Level vi, easy-to-eat food for 3 meals, simply alternative nutrition used; Level 7, like shooting fish in a barrel-to-eat food orally ingested in 3 meals with no culling nutrition given; Level eight, patient eats three meals, only excluding food that is especially difficult to swallow; Level 9, no dietary restriction, and patient ingesting three meals orally, with medical considerations; and Level 10, normal.
Radiographic measurements
We reviewed lateral evidently X-rays of the cervical spine under conditions of halo-vest fixation to measure O-C2 angle, C2-C6 angle, narrowest oropharyngeal airway infinite (nPAS) as an indicator of pharyngeal space [14], and pharyngeal inlet angle (PIA) [19] inside 2 days from FILS evaluation.
O-C2 angle was defined as the angle between McGregor'southward line (fabricated by cartoon a line connecting the posterior border of the difficult palate to the nigh caudal portion of the occipital bend) and the inferior endplate line of C2. C2-C6 angle was defined as the angle between the inferior endplate line of C2 and the inferior endplate line of C6. Positive values for both O-C2 and C2–C6 angles indicated lordosis at the measured segments [14]. The definition of nPAS was the narrowest anteroposterior distance of the oropharynx betwixt the tips of the uvula and epiglottis [14]. Finally, PIA was divers equally the bending between McGregor's line and the line fabricated by drawing a line connecting the center of the C1 anterior arch to the noon of the cervical sagittal curvature [19] (Fig. 1).
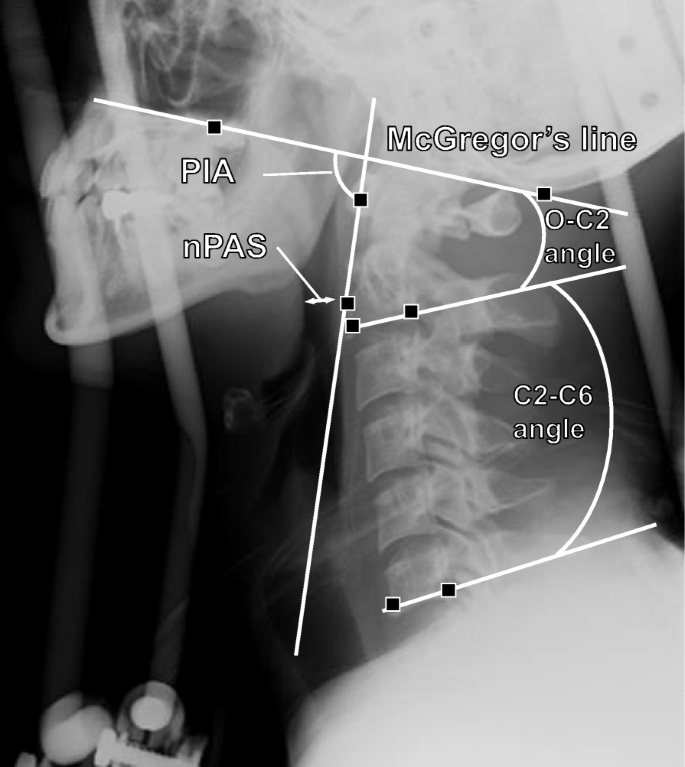
Representative lateral plain X-rays of the cervical spine. O-C2 bending is defined as the angle between McGregor's line (the line connecting the posterior edge of the hard palate to the most caudal portion of the occipital curve) and the inferior endplate line of C2. C2-C6 angle is defined as the angle between the inferior endplate line of C2 and the inferior endplate line of C6. The narrowest anteroposterior distance of the oropharynx between the tips of the uvula and epiglottis (double white arrow) is used every bit the nPAS. PIA represents the bending between McGregor'due south line and the line made by cartoon connecting the center of the C1 anterior arch to the apex of the cervical sagittal curvature
We also estimated soft-tissue swelling in the prevertebral area on lateral plain 10-rays of the cervical spine. Co-ordinate to a study by Rojas et al., which showed the normal range of thickness of prevertebral soft tissues, nosotros regarded thicknesses greater than 6 mm at C2, 7 mm at C3, or 18 mm at C6 on lateral plain 10-rays as representing prevertebral soft-tissue swellings [21].
We reviewed the presence or absenteeism of odontoid fracture, and the type of odontoid fracture every bit classified past Anderson and D'Alonzo [22]. Type 2 C2 fractures acquit a loftier chance of nonunion, and thus may bear upon functional outcomes in patients with halo-vest fixation [23].
Statistical analysis
Values are expressed as mean ± standard divergence and range. Differences in baseline characteristics were tested using the two-tailed t exam for continuous variables, the Mann-Whitney U test for non-normally distributed variables, and the χii test for categorical variables. Multivariate logistic analyses with forward pick based on likelihood ratio were used to evaluate the association between incidence of dysphagia and age, body mass index (BMI), ICU stay, and O-C2 angle, which were selected equally independent variables showing values of P < 0.ane in the two-tailed t examination, χii test, and Isle of man-Whitney test in Tabular array 1 (Model 1).
Moreover, the presence or absence of surgery for cervical fixation before halo-belong fixation, soft-tissue swelling in the prevertebral area, and days on ventilation, which were possible confounding factors for the incidence of dysphagia, were included as variables in addition to the variables in Model i for multivariate logistic analyses (Model two).
Spearman correlation coefficients were used to evaluate whether FILS level correlated with each independent factor identified in multivariate logistic analyses, and nPAS. Moreover, Pearson correlation coefficients were used to evaluate whether O-C2 angle correlated with C2-C6 angle, nPAS, or PIA. Values of P < 0.05 were considered statistically significant. We used SPSS version 17.0 software (SPSS, Chicago, IL) for all analyses.
Results
A total of 49 patients underwent halo-belong fixation in our institute between January 2006 and August 2016. Eight patients were excluded from this written report: 5 patients suffered from spinal cord injury classed as Grade A or B according to the Frankel classification; and 1 patient failed to show C2-C6 on lateral plainly X-rays due to obesity; and 2 patients suffered from facial trauma. Data from a full of 41 patients were analyzed.
For the total cohort, age was 59.2 ± 19.6 years, height was 160.ii ± ix.9 cm, weight was 58.five ± 13.9 kg, BMI was 22.seven ± 4.2 kg/mtwo, duration of wearing the halo-belong was 56.v ± 25.6 days, length of ICU stay was 0.59 ± i.46 days, elapsing of ventilator apply was 1.78 ± four.02 days, 10 patients underwent cervical fusion before halo-vest fixation, and 11 patients showed prevertebral soft-tissue swelling. Etiology of halo-vest fixation was trauma (n = 24), cervical spondylosis (n = v), suppurative spondylitis (due north = four), ossification of the posterior longitudinal ligament (n = 3) and other weather (north = five; 2 patients with rheumatoid arthritis, 1 patient with idiopathic cervical dislocation, 1 patient with metastatic carcinoma, and 1 patient with attempted suicide past hanging).
Based on FILS scoring, 13 patients (32%) suffered dysphagia during halo-vest fixation. Comparisons of clinical data from medical charts between non-dysphagia and dysphagia groups are shown in Table i. No meaning differences in sex, duration of wearing the halo-vest, duration of ventilator use, proportion of patients with tracheostomy, proportion of patients with cervical fusion earlier halo-vest fixation, proportion of patients with prevertebral soft-tissue swelling, the reason for halo-vest fixation, and complications were seen between non-dysphagia and dysphagia groups. Withal, historic period and length of ICU stay were significantly greater in the dysphagia group than in the not-dysphagia grouping (p = 0.044, 0.013, respectively). BMI tended to exist greater in the dysphagia group than in the non-dysphagia group (p = 0.055).
Twelve patients (29%) were diagnosed with odontoid fracture, comprising Anderson and D'Alonzo type II in three patients, and blazon 3 in nine patients [22]. No difference in type of odontoid fracture was seen between non-dysphagia and dysphagia groups.
In radiographic information for all subjects, O-C2 angle was 16.four ± ix.5°, C2-C6 bending was thirteen.0 ± ten.7°, nPAS was 13.5 ± 5.half dozen mm and PIA was 91.1 ± 8.5°. Comparisons of radiographic measurements betwixt not-dysphagia and dysphagia groups are shown in Table 2. O-C2 bending was significantly smaller in the dysphagia grouping than in the non-dysphagia group. On the other mitt, C2-C6 angle, nPAS and PIA did non differ significantly between groups.
Results of multivariate logistic analyses using age, BMI, ICU stay, and O-C2 angle as covariates (Model one) are shown in Tabular array 3. BMI (odds ratio [OR] 0.59, 95% confidence interval [CI] 0.38–0.93, p = 0.024), ICU stay (OR iii.68, 95%CI one.27–10.62, p = 0.016), and O-C2 angle (OR 0.83, 95%CI 0.71–0.97, p = 0.021) remained independent chance factors related to incidence of dysphagia.
Moreover, in the logistic analyses, we added presence or absence of operation for cervical fixation before halo-vest fixation, soft-tissue swelling in the prevertebral surface area, and days on ventilation as covariates, equally these were also possible confounding factors for the incidence of dysphagia (Model ii). However, no differences in statistical results were constitute between Models 1 and 2.
A negative correlation was seen between ICU stay and FILS level (r = 0.348, p = 0.026; Fig. 2a). No pregnant correlation was seen between BMI and FILS level (Fig. 2b). A positive correlation was seen between O-C2 angle and FILS level (r = 0.411, p = 0.008; Fig. 2c). No significant correlation was seen betwixt nPAS and FILS level (r = 0.272, p = 0.085) (information not shown).
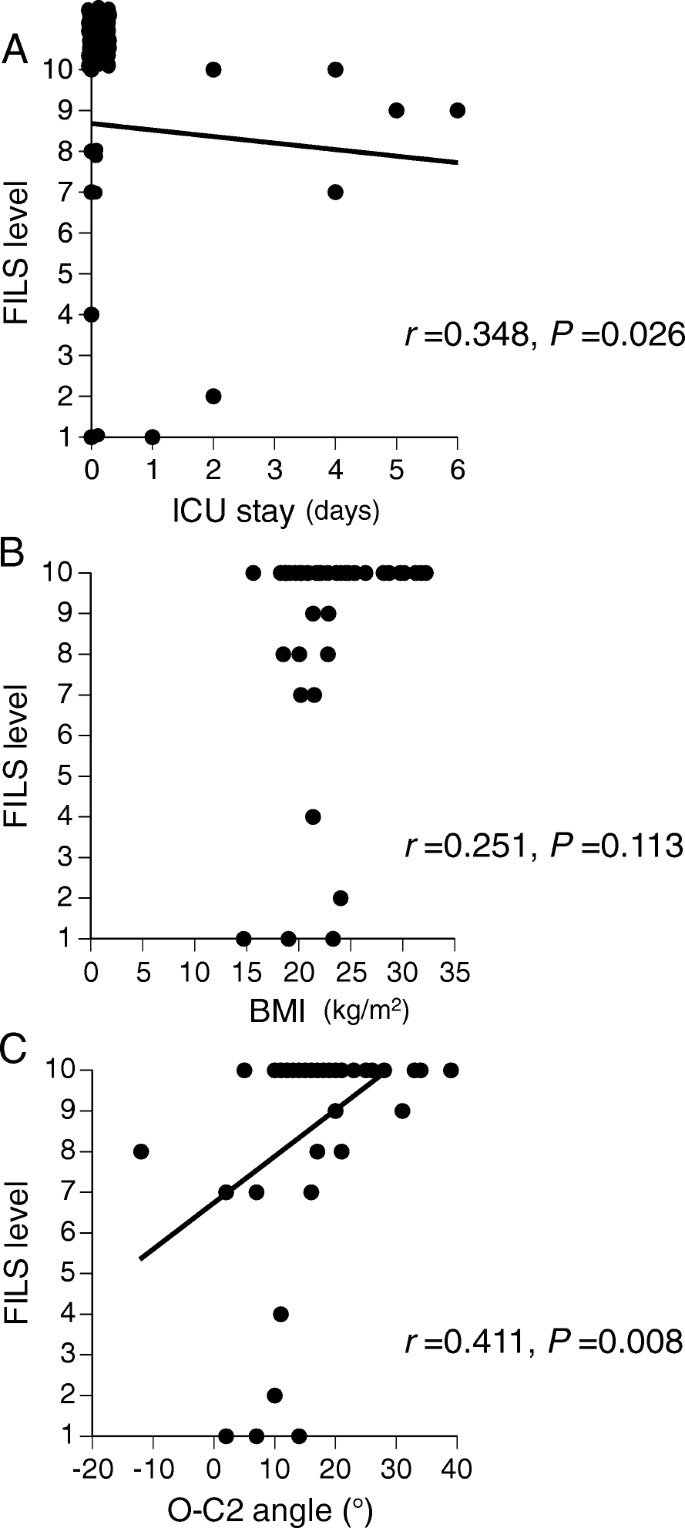
a Scatter diagram showing association of ICU stay and FILS level. b Scatter diagram showing association of BMI and FILS level. c Scatter diagram showing association of O-C2 bending and FILS level
A negative correlation was seen between O-C2 and C2-C6 angles (r = 0.498, p = 0,001; Fig. 3a). A positive correlation was seen betwixt O-C2 bending and nPAS (r = 0.468, p = 0.002; Fig. 3b). A positive correlation was also seen between O-C2 angle and PIA (r = 0.738, p < 0.001; Fig. 3c). The coefficient ratio (η) for incidence of dysphagia was 0.373, 0.117, 0.167, and 0.109 for O-C2 bending, C2-C6 angle, nPAS, and PIA, respectively.
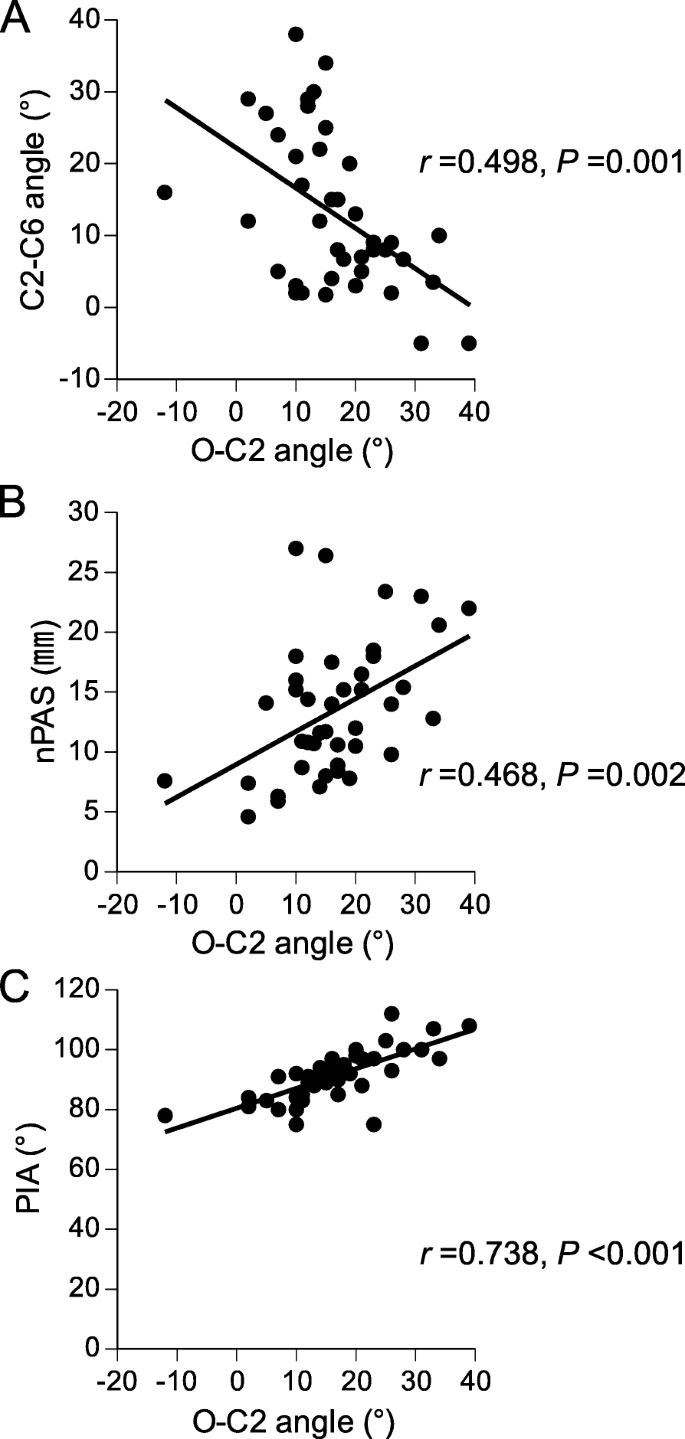
a Scatter diagram showing clan of O-C2 and C2-C6 angles. b Scatter diagram showing clan of O-C2 angle and nPAS. c Scatter diagram showing association of O-C2 angle and PIA
Discussion
Although previous studies have identified dysphagia every bit a complication of halo-vest fixation, cervical alignment has not been investigated as a crusade of dysphagia in patients treated with a halo-vest brace. The nowadays study identified ICU stay, BMI, and O-C2 bending as independent risk factors for the incidence of dysphagia among patients with halo-vest fixation. Furthermore, we constitute that both smaller O-C2 bending and longer ICU stay were associated with lower FILS level.
We reviewed 41 patients who had undergone halo-belong fixation. The mean age of all patients was 59.ii years, older than patients in previous studies (range, 28.3–43 years). The proportion of male subjects in our written report was 59%, consequent with previous studies [24,25,26]. In terms of causative factors, 59% of patients showed a traumatic etiology. Using clinical data from medical charts, we found that age and elapsing of ICU stay were greater in the dysphagia group than in the non-dysphagia group.
Bradley et al. [6] retrospectively reviewed 56 patients treated with a halo-belong due to traumatic cervical fracture. In that study, the rate of dysphagia was much higher (66%) than in our study (32%), presumably because our subjects included not-traumatic patients. The proportion of males in their dysphagia group (65%) was consistent with our observations (62%). The study showed that ICU stay was longer in patients with dysphagia and was associated with severity of dysphagia, consistent with our findings.
We revealed O-C2 angle as a gene independently associated with the incidence of dysphagia among patients with halo-vest fixation, and smaller O-C2 angle was related to lower FILS level. On the other hand, C2-C6 bending did not differ significantly betwixt groups. Previous studies in patients who had undergone cervical fusion involving the cranium showed that O-C2 angle was related to the incidence of dysphagia [vii,8,9,x,xi,12,xiii,fourteen,15,16]. Since the halo-vest is most effective method of fixation for vertebrae of the upper cervical spine, halo-vest fixation may resemble cervical fusion with the attic rather than that without the cranium.
In this study, nPAS did not differ significantly between groups, and no significant correlation was evident between nPAS and FILS level, fifty-fifty though a positive correlation was seen betwixt O-C2 angle and nPAS (Fig. 3b). This event suggests that O-C2 angle may affect not only the pharyngeal infinite, but also other factors related to dysphagia in patients with halo-vest fixation. In addition, PIA did not differ betwixt patients with and without dysphagia. Taken together, narrowing of the pharyngeal space may not be crucial for the development of dysphagia during halo-vest fixation. Further studies are required to elucidate the relationship between O-C2 bending and incidence of dysphagia during halo-belong fixation.
BMI did non differ significantly between groups. Still, BMI remained independently associated with dysphagia amidst patients with halo-belong fixation according to logistic analysis. Maeda et al. [27] reviewed 224 elderly inpatients with and without dysphagia. They reported that the BMI of patients was lower in the dysphagia group than in the non-dysphagia group, consequent with our results. Since they revealed sarcopenia as an independent risk factor for dysphagia in hospitalized elderly individuals, our patients with dysphagia may take suffered from sarcopenia [27].
Figure 2c suggests several clinical issues worthy of consideration. First, the divergence of five° in O-C2 angle resulted in a deviation of 1 point in the FILS score, suggesting the usefulness of describing the radiographic bending measurement compared to gaze angle or gross clinical appearance. At the time of halo-vest assembly, lateral cervical spine X-ray including the skull to ensure an adequate O-C2 bending may be helpful in finding the best position to permit normal swallowing in patients with halo-vest fixation. Previously, the recommendation for positioning in halo-vest fixation to maintain normal swallowing physiology has been but to avoiding cervical hyperextension [5]. In this study, nosotros revealed another important issue of positioning to forestall dysphagia in halo-vest fixation.
When we perform halo-belong fixation, we pay attention to fixing the spine in a cervical neutral position nether X-ray fluoroscopic imaging. Among the 130° of total flexion-extension range of move of the neck, but 20–thirty° (xv–25%) is involved in O-C2 articulations [28]. The positioning therefore usually occurs through the lower cervical spine, and variance in C2–6 becomes low. O-C2 angle is non commonly given much attention during the process for halo-vest fixation. However, we found that O-C2 angle was significant in patients with halo-belong fixation to preclude dysphagia.
Figure 3a and c show that O-C2 angle correlated significantly with both C2-C6 angle and PIA, suggesting the beingness of collinearity amidst each of the radiographic measurement items investigated in the study. The coefficient ratios suggested that O-C2 angle may provide the greatest contribution to the incidence of dysphagia among the items examined. However, other components of occipitocervical alignment such as translation forward or back in the horizontal aeroplane and/or angulation at dissimilar areas of cervical spine may also impact the incidence of dysphagia. Further studies are warranted to analyze other radiographic measurement items affecting swallowing functions.
This study had several limitations, including the retrospective report design. In add-on, fiberoptic endoscopic and/or video-fluoroscopic swallow studies were not performed for every patient. Some other limitation was the lack of radiographic data before halo-belong fixation. Nosotros were therefore unable to evaluate changes in alignment, which might exist more relevant than angles at a single time betoken.
Conclusions
In this study, O-C2 angle was significantly smaller in patients who developed dysphagia during halo-belong fixation. BMI, ICU stay, and O-C2 angle were contained run a risk factors for dysphagia in patients with halo-belong fixation. Moreover, smaller O-C2 angle and longer ICU stay were associated with lower FILS. These results suggest that inadequate extension at O-C2 may contribute to swallowing difficulties in patients with halo-vest fixation.
Availability of data and materials
The datasets used and/or analyzed during electric current study are bachelor from the corresponding author on reasonable asking.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- FILS:
-
Food intake level scale
- ICU:
-
Intensive care unit
- nPAS:
-
Narrowest oropharyngeal airway space
- O-C2 bending:
-
Occipito-C2 bending
- OPLL:
-
Ossification of posterior longitudinal ligament
- OR:
-
Odds ratio
- PIA:
-
Pharyngeal inlet angle
References
-
Johnson RM, Hart DL, Simmons EF, Ramsby GR, Southwick WO. Cervical orthoses. A study comparison their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg Am. 1977;59(three):332–9.
-
Karimi MT, Kamali G, Fatoye F. Evaluation of the efficiency of cervical orthoses on cervical fracture: a review of literature. J Craniovertebr Junction Spine. 2016;7(1):thirteen–9.
-
Koch RA, Nickel VL. The halo belong: an evaluation of motion and forces beyond the neck. Spine (Phila Pa 1976). 1978;3(2):103–7.
-
Taitsman LA, Altman DT, Hecht AC, Pedlow FX. Complications of cervical halo-vest orthoses in elderly patients. Orthopedics. 2008;31(5):446.
-
Morishima North, Ohota M, Miura Y. The influences of halo-vest fixation and cervical hyperextension on swallowing in healthy volunteers. Spine (Phila Pa 1976). 2005;30(7):E179–82.
-
Bradley JF 3rd, Jones MA, Farmer EA, Fann SA, Bynoe R. Swallowing dysfunction in trauma patients with cervical spine fractures treated with halo-belong fixation. J Trauma. 2011;seventy(1):46–8 give-and-take 48-50.
-
Ebata S, Hatsushika G, Ohba T, Nitta K, Akaike H, Masuyama Thousand, et al. Swallowing function later occipitocervical arthrodesis for cervical deformity in patients with rheumatoid arthritis. NeuroRehabilitation. 2015;37(ii):299–304.
-
Izeki M, Neo Grand, Takemoto M, Fujibayashi Due south, Ito H, Nagai Grand, et al. The O-C2 angle established at occipito-cervical fusion dictates the patient's destiny in terms of postoperative dyspnea and/or dysphagia. Eur Spine J. 2014;23(2):328–36.
-
Kaneyama S, Sumi M, Kasahara K, Kanemura A, Takabatake One thousand, Yano T. Dysphagia after Occipitothoracic fusion is caused past direct compression of Oropharyngeal infinite due to anterior protrusion of mid-cervical spine. Clin Spine Surg. 2017;30(vii):314–20.
-
Meng Y, Wu T, Liu Z, Wen D, Rong 10, Chen H, Lou J, Liu H. The impact of the difference in O-C2 angle in the development of dysphagia after occipitocervical fusion: a simulation study in normal volunteers combined with a example-control written report. Spine J. 2018;18(viii):1388–97.
-
Miyata M, Neo Yard, Fujibayashi Due south, Ito H, Takemoto M, Nakamura T. O-C2 angle as a predictor of dyspnea and/or dysphagia subsequently occipitocervical fusion. Spine (Phila Pa 1976). 2009;34(2):184–viii.
-
Wang X, Chou D, Jian F. Influence of postoperative O-C2 bending on the development of dysphagia after Occipitocervical fusion surgery: results from a retrospective assay and prospective validation. World Neurosurg. 2018;116:e595–601.
-
Yoshida M, Neo Yard, Fujibayashi S, Nakamura T. Upper-airway obstruction after short posterior occipitocervical fusion in a flexed position. Spine (Phila Pa 1976). 2007;32(viii):E267–70.
-
Ota One thousand, Neo M, Aoyama T, Ishizaki T, Fujibayashi South, Takemoto K, et al. Affect of the O-C2 angle on the oropharyngeal infinite in normal patients. Spine (Phila Pa 1976). 2011;36(11):E720–6.
-
Kaneyama South, Sumi Grand, Takabatake M, Kasahara K, Kanemura A, Koh A, et al. Preliminary evaluation of the Pathomechanisms of dysphagia later on Occipitospinal fusion: kinematic analysis by Videofluoroscopic swallowing study. Spine (Phila Pa 1976). 2016;41(23):1777–84.
-
Kawamura I, Tominaga H, Tanabe F, Yamamoto T, Taniguchi N. Cervical alignment of anterior cervical hyperostosis causing dysphagia. Spine (Phila Pa 1976). 2019;44(5):E269–72.
-
Tian W, Yu J. The role of C2-C7 and O-C2 bending in the development of dysphagia subsequently cervical spine surgery. Dysphagia. 2013;28(two):131–8.
-
Tian Westward, Yu J. The role of C2-C7 angle in the development of dysphagia later on anterior and posterior cervical spine surgery. Clin Spine Surg. 2017;30(9):E1306–14.
-
Kaneyama S, Sumi K, Takabatake Chiliad, Kasahara K, Kanemura A, Hirata H, et al. The prediction and prevention of dysphagia after Occipitospinal fusion by use of the S-line (swallowing line). Spine (Phila Pa 1976). 2017;42(x):718–25.
-
Kunieda Yard, Ohno T, Fujishima I, Hojo Thousand, Morita T. Reliability and validity of a tool to mensurate the severity of dysphagia: the food intake LEVEL scale. J Hurting Symptom Manag. 2013;46(2):201–half-dozen.
-
Rojas CA, Vermess D, Bertozzi JC, Whitlow J, Guidi C, Martinez CR. Normal thickness and appearance of the prevertebral soft tissues on multidetector CT. AJNR Am J Neuroradiol. 2009;30(1):136–41.
-
Anderson LD, D'Alonzo RT. Fractures of the odontoid process of the axis. J Os Joint Surg Am. 1974;56(eight):1663–74.
-
Girardo Chiliad, Rava A, Gargiulo K, Coniglio A, Artiaco S, Masse A, et al. Clinical and radiological union charge per unit evaluation of type 2 odontoid fractures: a comparison between anterior screw fixation and halo vest in elderly patients. J Craniovertebr Junction Spine. 2018;ix(iv):254–9.
-
Garfin SR, Botte MJ, Waters RL, Nickel VL. Complications in the use of the halo fixation device. J Bone Joint Surg Am. 1986;68(three):320–5.
-
Kim DH, Vaccaro AR, Affonso J, Jenis L, Hilibrand AS, Albert TJ. Early predictive value of supine and upright X-ray films of odontoid fractures treated with halo-vest immobilization. Spine J. 2008;8(4):612–8.
-
Rockswold GL, Bergman TA, Ford SE. Halo immobilization and surgical fusion: relative indications and effectiveness in the treatment of 140 cervical spine injuries. J Trauma. 1990;thirty(7):893–8.
-
Maeda K, Akagi J. Sarcopenia is an independent risk factor of dysphagia in hospitalized older people. Geriatr Gerontol Int. 2016;16(4):515–21.
-
Kapandji AI. Physiology of the joints, vol. three. 6th ed. Paris: Maloin; 2017. p. P232–3.
Acknowledgements
Not applicable.
Funding
This study was supported past Grants-in-Aid for Scientific Research from the Japanese Ministry of Teaching, Civilisation, Sports, Science and Technology (grant numbers 24300187, 24659397, 26460899, 15 K12588, xv K15254, 15 K01420, xv K11644, 19H03984, and 19 K22821 to S.E.), Research Funding for Longevity Sciences (25–7, 28–13 to S.E.) from the Japanese National Center for Geriatrics and Gerontology, the Research Promotion Grant from Toho University Graduate School of Medicine (No.17–04 to S.East.), the Project Inquiry Grant from Toho Academy School of Medicine (No.xix–22 to Thou.M.) and a Enquiry Grant from the Japanese Order of Dysphagia Rehabilitation (to M.Thousand.). The funders have no role in the pattern of the study and collection, analysis, and interpretation of information and in writing the manuscript.
Author information
Affiliations
Contributions
M.M. and S.East. designed the study, participated in the study, conducted acquisition, assay, and interpretation of information, and drafted the manuscript. H.T., Thousand.T. and H.South. helped design the study, participated in the report, and conducted acquisition, analysis, and interpretation of data. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the upstanding standards of the institutional and/or national enquiry committee and with the 1964 Annunciation of Helsinki and its subsequently amendments. The study protocol was approved by the Ethics Committee of Toho Academy Omori Medical Center (No. 27–279). Informed consent was obtained from all individual participants included in this retrospective study by the opt-out consent procedure.
Consent for publication
Not applicable.
Competing interests
The authors declare that they accept no competing interests.
Additional information
Publisher's Annotation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Eatables Attribution iv.0 International License, which permits use, sharing, accommodation, distribution and reproduction in any medium or format, as long as yous give appropriate credit to the original author(s) and the source, provide a link to the Creative Eatables licence, and signal if changes were made. The images or other third party cloth in this commodity are included in the article's Artistic Commons licence, unless indicated otherwise in a credit line to the cloth. If material is not included in the article'due south Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, y'all will demand to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/null/one.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and Permissions
About this article
Cite this article
Miyagi, M., Takahashi, H., Tsuchiya, K. et al. Role of O-C2 angle in the development of dysphagia in patients with halo-vest fixation. BMC Musculoskelet Disord 21, 131 (2020). https://doi.org/10.1186/s12891-020-3155-2
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s12891-020-3155-2
Keywords
- Halo-vest
- Dysphagia
- O-C2 angle
- Food intake level
Source: https://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/s12891-020-3155-2
0 Response to "2. Apply Baby Powder Under the Halo Vest to Prevent Irritation."
Post a Comment